Tardive dyskinesia (TD) is a persistent hyperkinetic movement disorder caused by prolonged exposure to dopamine receptor blocking agents, including antipsychotics.1-3 Even mild TD movements can significantly impact various aspects of patients’ lives, extending into the social, psychological, and emotional domains.4,5 The American Psychiatric Association (APA) Guidelines recommend vesicular monoamine transporter 2 (VMAT2) inhibitors, like AUSTEDO XR, for treating TD if it has an impact on the patient, regardless of severity of movements.6,7 The goal of this article is to inform advanced practice providers on how to treat TD by offering an overview of AUSTEDO XR, a once-daily treatment option for adults with this disorder. To that end, key efficacy and safety data from the pivotal clinical trials with AUSTEDO are presented. This article further highlights real-world evidence from a survey assessing patients’ experiences with AUSTEDO XR and reviews recommendations and considerations for patients taking concomitant medications, as well as AUSTEDO XR dosing options.
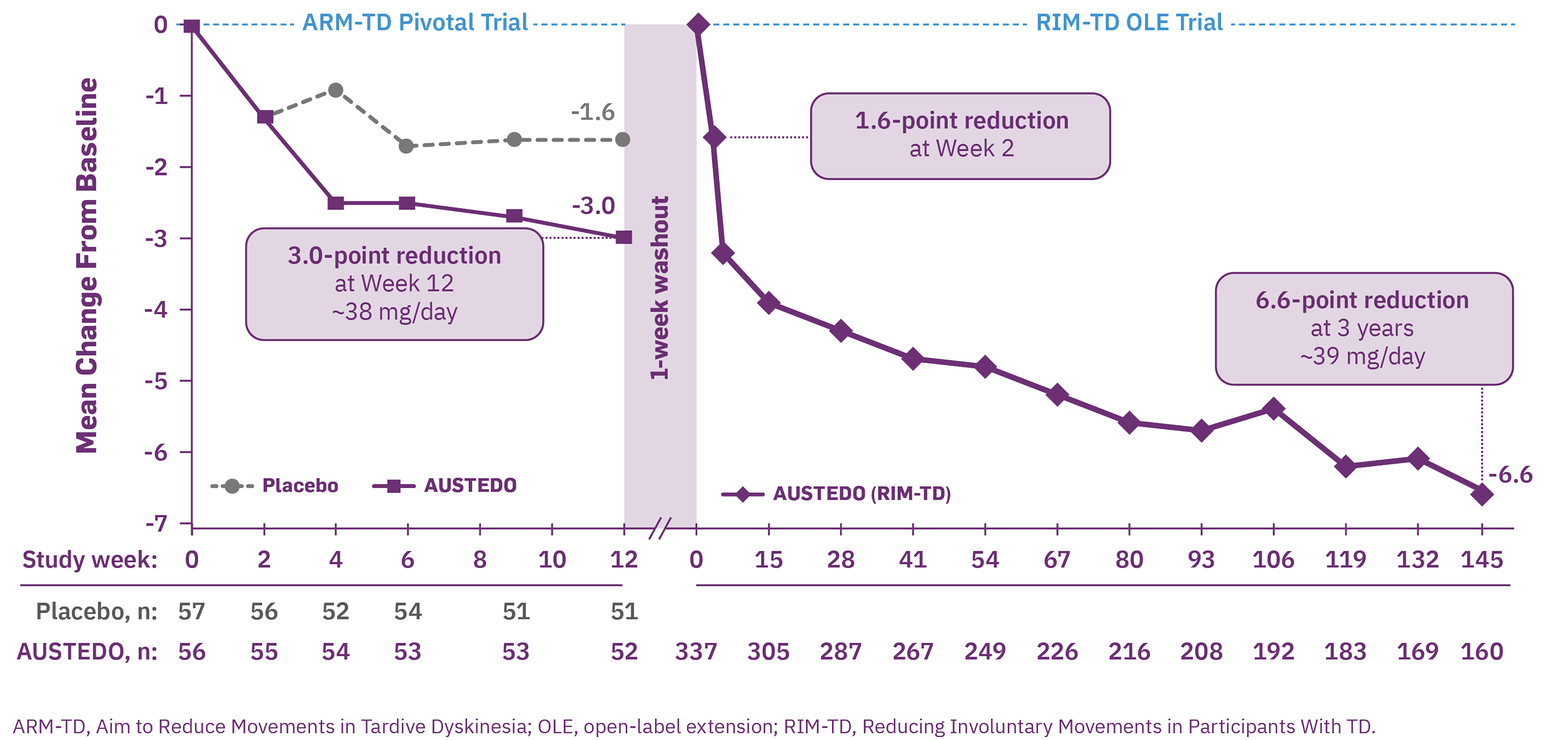
The efficacy and safety of AUSTEDO in the treatment of TD was evaluated in 2 pivotal clinical trials, ARM-TD (Aim to Reduce Movements in Tardive Dyskinesia) and AIM-TD (Addressing Involuntary Movements in Tardive Dyskinesia).8,9
- ARM-TD was a 12-week, randomized, double-blind, placebo-controlled trial in which doses were titrated to an individualized dose that reduced abnormal movements and was tolerated. After screening, patients were randomized 1:1 to receive AUSTEDO twice daily (BID) or placebo9
- AIM-TD was a 12-week, randomized, double-blind, placebo-controlled trial in which patients received AUSTEDO 0 mg (placebo), 12 mg/day, 24 mg/day, or 36 mg/day.7,8
The primary efficacy endpoint in both trials was the change in Abnormal Involuntary Movement Scale (AIMS) total score from baseline to Week 12.7-10
RIM-TD (Reducing Involuntary Movements in Participants With TD), an open-label study, was designed to evaluate long-term treatment with AUSTEDO for up to 3 years following completion of ARM-TD or AIM-TD. Among the patients evaluated, 337 patients were in treatment at baseline and 160 patients remained on treatment through the end of Week 145.11 The mean overall compliance rate was nearly 90% at 3 years.10
In the placebo-controlled trials, patients who received AUSTEDO demonstrated a rapid response as early as Week 2 and achieved a significant and meaningful reduction in TD severity at Week 12.7,9,10
- In ARM-TD, patients receiving AUSTEDO demonstrated a statistically significant improvement in AIMS total score, with a reduction of 3.0 points from baseline to Week 12, compared with 1.6 points in the placebo group (treatment effect of -1.4 points, P=0.019) (Figure 1, left graph).9.10 At Week 12, 94% of patients were taking a dose of ≥30 mg/day, and the average daily dose was ~38 mg9,10
- In AIM-TD, AUSTEDO significantly reduced AIMS total score by 3.3 points from baseline in the 36 mg/day arm compared with a reduction of 1.4 points with placebo at Week 12 (treatment effect of -1.9 points, P=0.001).7,8 The average daily dose was ~39 mg.8
In the open-label extension (OLE) study, increased improvement in AIMS total score was observed over 3 years, with 71% of patients at Week 145 seeing improvement relative to Week 15 (Figure 1, right graph).10,11 At Week 145, 87% of patients were taking a dose of ≥30 mg/day and the average daily dose was ~39 mg.10,11
The most common adverse reactions reported across both placebo-controlled studies in patients with TD treated with AUSTEDO (>3% and greater than placebo) were nasopharyngitis and insomnia.7 Adverse reactions occurring in patients treated with AUSTEDO (12-48 mg/day) (≥2%) are summarized in Figure 2.
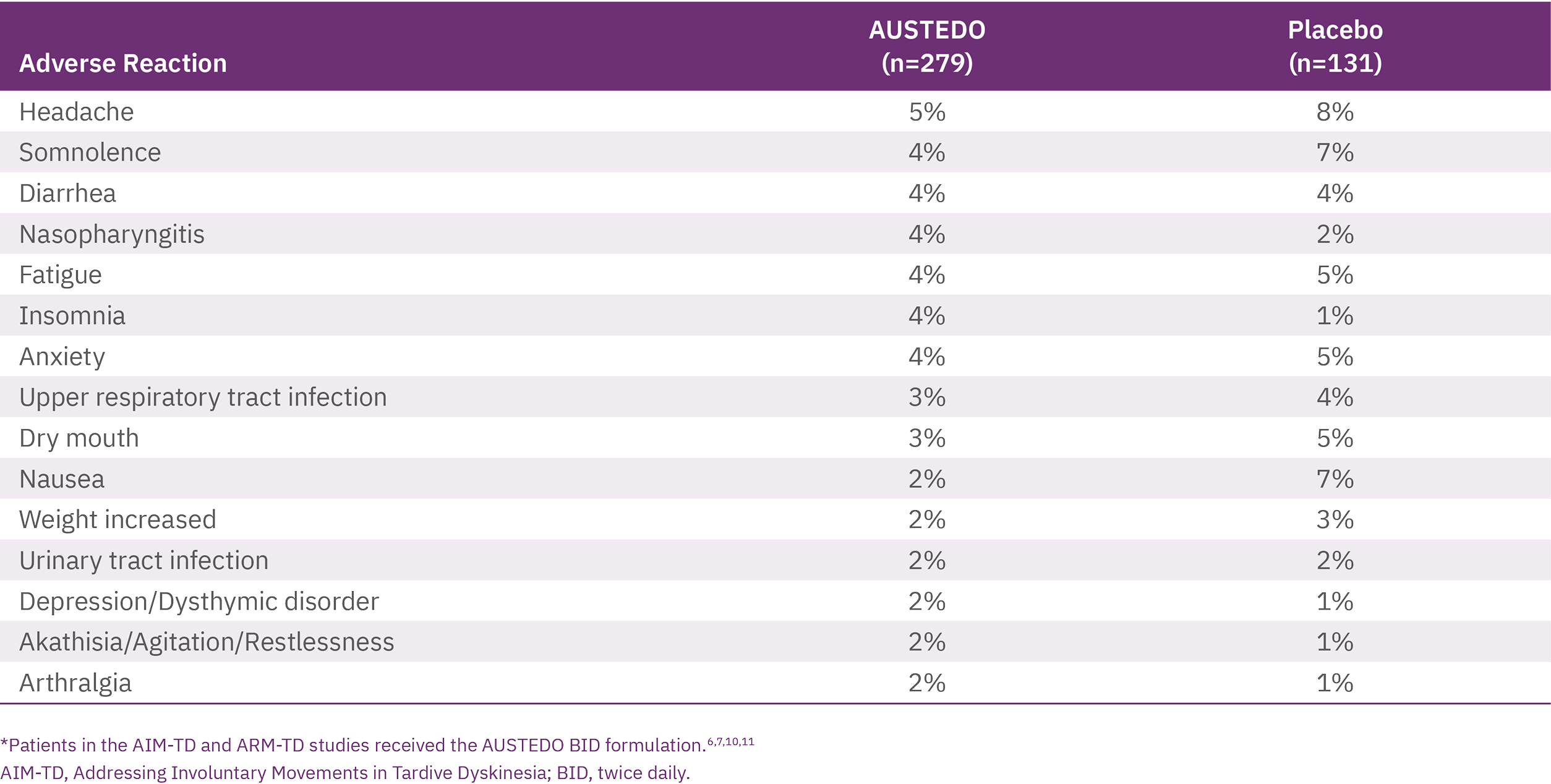
Discontinuation due to adverse events (AEs) occurred in 4% of patients compared with 3% of patients treated with placebo.8 Four percent of patients required dose reduction of AUSTEDO due to AEs compared with 2% of patients taking placebo.7 Once patients were titrated to their maintenance dose, several AEs were no longer reported, including dry mouth and nausea in AIM-TD and somnolence and dry mouth in ARM-TD.10
No new safety signals were identified in RIM-TD, and AEs were comparable with those in the 12-week clinical trials.11
Adverse reactions with AUSTEDO XR are expected to be similar to AUSTEDO BID.7
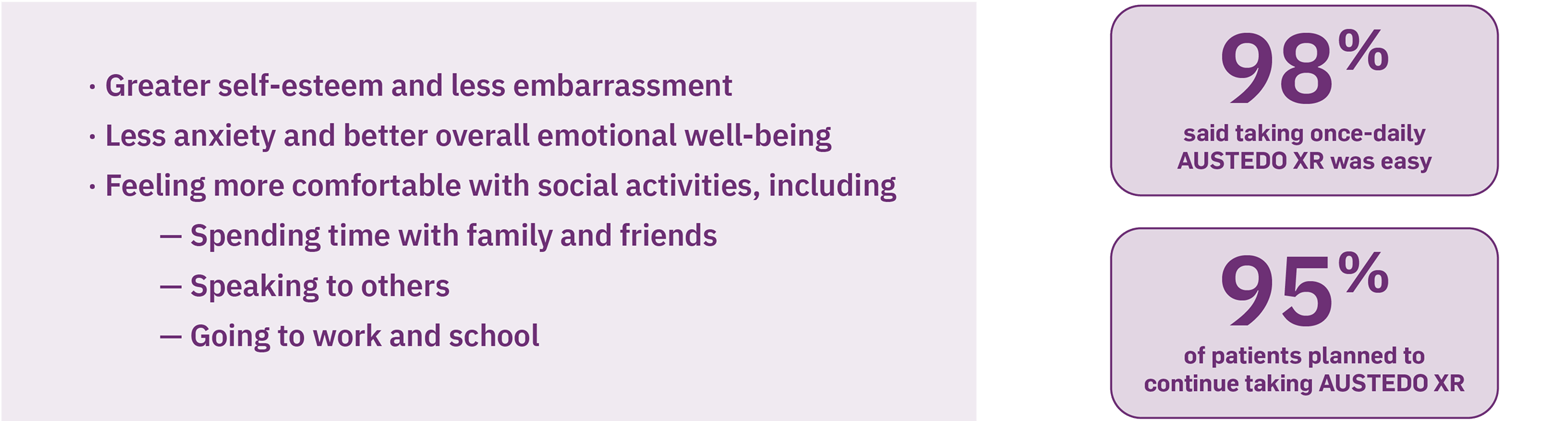
In addition to clinical data, real-world evidence of patient-reported experiences may help inform discussions about treatment with your patients. This was highlighted in a prospective, cross-sectional survey involving 118 patients with TD, which assessed patients’ experiences with AUSTEDO XR, including perceived ease of use and effects on social and emotional well-being. Interim results from this survey found that more than 50% of patients reported improved social and emotional well-being as a result of movement reduction with AUSTEDO XR. Patients reported greater self-esteem (66%), less embarrassment (73%) and anxiety (59%), and better overall emotional well-being (77%) (Figure 3). In addition, 98% of patients said taking once-daily AUSTEDO XR was easy, and 95% planned to continue taking AUSTEDO XR (Figure 3). Furthermore, 86% liked the ability to adjust their dose up or down with their doctor and >60% reported taking AUSTEDO XR in the morning.12
Patients with TD may also be taking medications to treat nonpsychiatric comorbidities in addition to medication to stabilize their mental health condition. In order to reduce the risk of drug-drug interactions, it is critical that clinicians are aware of the patient’s medication regimen and consider metabolic pathways when selecting a VMAT2 inhibitor to treat TD. AUSTEDO XR is metabolized primarily by CYP2D6, with minor contributions from CYP3A4/5 and other enzymes to form several minor metabolites.7 When potential drug interactions with CYP3A4 or CYP2D6 are considered, AUSTEDO XR offers flexibility with several dosing options, allowing adjustments up to 36 mg/day (Figure 4).7 Moreover, no dose adjustments to P-glycoprotein substrates (eg, calcium channel blockers, statins, and antimicrobials) are required when taking AUSTEDO XR.7,13
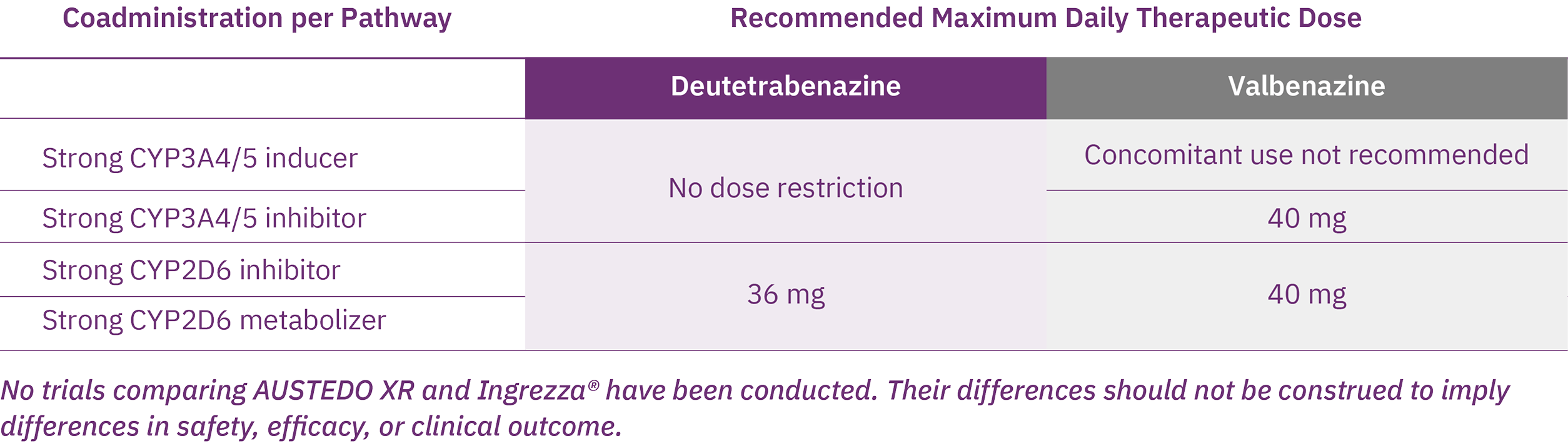
AUSTEDO XR is the only VMAT2 inhibitor indicated for TD with no dose restrictions for—or recommendations against— concomitant use with strong CYP3A4/5 inducers or inhibitors7,14
AUSTEDO XR offers a variety of therapeutic doses, providing flexibility to achieve effective and tolerable symptom control.7 The recommended starting dose of AUSTEDO XR for patients with TD is 12 mg/day, which may be increased at weekly intervals by 6 mg/day.7 The average daily dose in clinical trials was >36 mg/day, and 52% of patients were taking between 36 mg/day and 48 mg/day at Week 145 in the long-term study.8,11 In separate pharmacokinetic studies, increased plasma levels of AUSTEDO correlated with higher potential for treatment success, but not AEs.15,16
AUSTEDO XR should be swallowed whole. Tablets should not be chewed, crushed, or broken. AUSTEDO XR may be taken with or without food (Figure 5).7
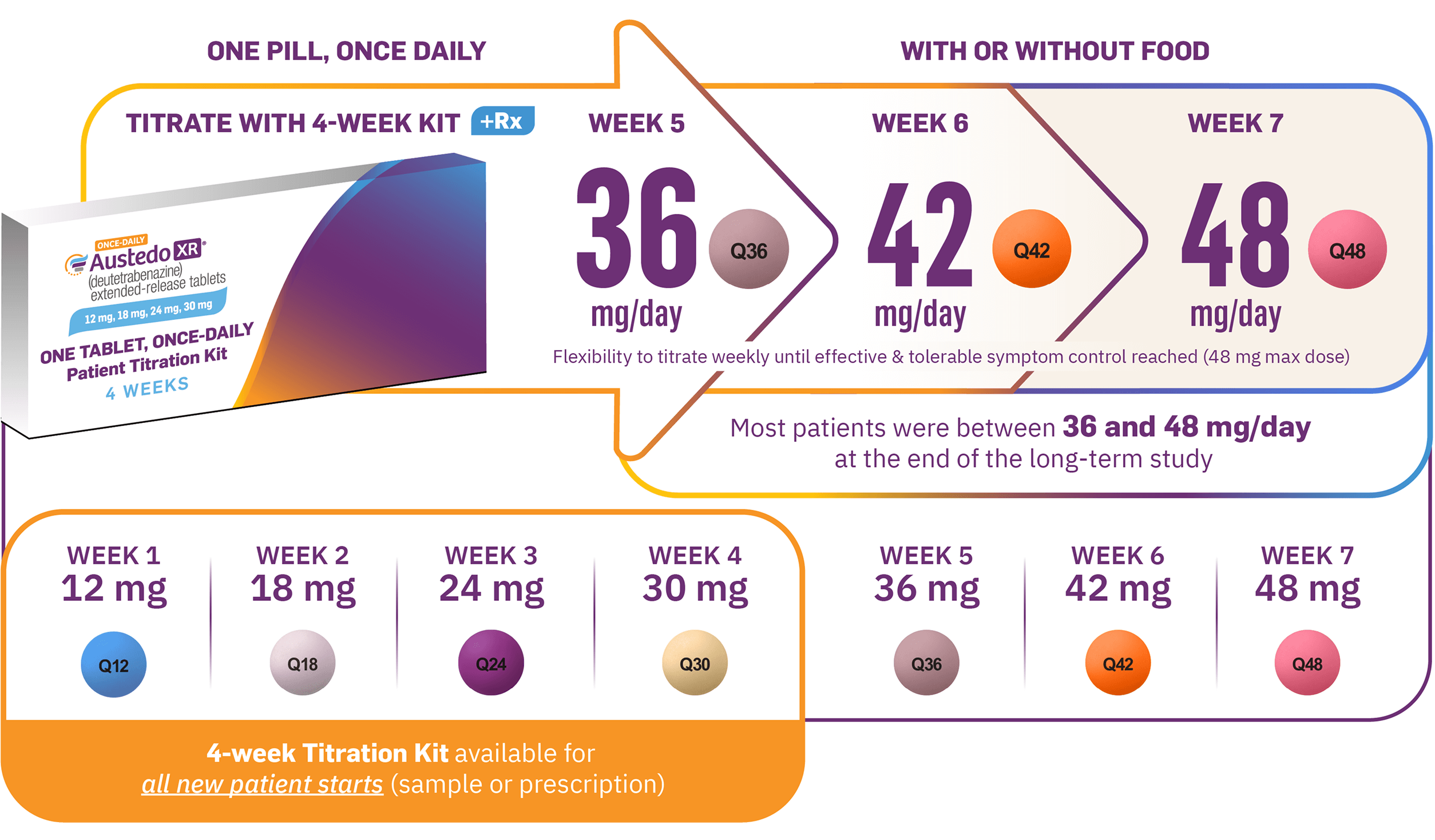
Image shown is not the actual 4-week Titration Kit. Tablets not shown to actual size.
- Patients treated with AUSTEDO in the ARM-TD and AIM-TD placebo-controlled studies achieved significant and meaningful reduction in TD severity at Week 127-9
- Increasing improvement in AIMS score was observed over 3 years in RIM-TD, with 71% of patients at Week 145 seeing improvement relative to Week 1510,11
- The most common AEs for AUSTEDO (3% and greater than placebo) in placebo-controlled studies in patients with TD were nasopharyngitis and insomnia. Adverse reactions with AUSTEDO XR are expected to be similar to AUSTEDO7
- Additionally, patients expressed satisfaction with the convenience of AUSTEDO XR as a once-daily tablet, appreciating the flexibility of taking it with or without food and at various times throughout the day12
- The flexible, once-daily dosing with AUSTEDO XR enables patients to titrate as needed to achieve effective and tolerable symptom control7
1. Hauser RA, Meyer JM, Factor SA, et al. Differentiating tardive dyskinesia: a video-based review of antipsychotic-induced movement disorders in clinical practice. CNS Spectr. 2022;27(2):208-217. 2. Fahn S, Jankovic J, Hallett M, eds. Principles and Practice of Movement Disorders. 2nd ed. Elsevier, Inc; 2011. 3. Zutshi D, Cloud LJ, Factor SA. Tardive syndromes are rarely reversible after discontinuing dopamine receptor blocking agents: experience from a university-based movement disorder clinic. Tremor Other Hyperkinet Mov (N Y). 2014;4:266. 4. Jackson R, Brams MN, Carlozzi NE, et al. Impact-Tardive Dyskinesia (Impact-TD) scale: a clinical tool to assess the impact of tardive dyskinesia. J Clin Psychiatry. 2022;84(1):22cs14563. 5. Finkbeiner S, Konings M, Henegar M, et al. Interim analysis of a patient-reported impact measure in the IMPACT-TD Registry. Presented at: Annual Psych Congress Elevate; May 30-June 2, 2024; Las Vegas, NV. 6. American Psychiatric Association. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia. 3rd ed. Washington, DC: American Psychiatric Association; 2021. Accessed March 25, 2025. https://psychiatryonline.org/doi/pdf/10.1176/appi.books.9780890424841 7. AUSTEDO XR® (deutetrabenazine) extended-release tablets/AUSTEDO® current Prescribing Information. Parsippany, NJ: Teva Neuroscience, Inc. 8. Anderson KE, Stamler D, Davis MD, et al. Deutetrabenazine for treatment of involuntary movements in patients with tardive dyskinesia (AIM-TD): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Psychiatry. 2017;4(8):595-604. 9. Fernandez HH, Factor SA, Hauser RA, et al. Randomized controlled trial of deutetrabenazine for tardive dyskinesia: the ARM-TD study. Neurology. 2017;88(21):2003-2010. 10. Data on file. Teva Neuroscience, Inc. Parsippany, NJ. 11. Hauser RA, Barkay H, Fernandez HH, et al. Long-term deutetrabenazine treatment for tardive dyskinesia is associated with sustained benefits and safety: a 3-year, open-label extension study. Front Neurol. 2022;13:773999. 12. Jain R, Konings M, Thompson S, Yang A, Kotak S, Gandhi P. Real-world evidence of patient experience with once-daily deutetrabenazine extended-release tablets for tardive dyskinesia and chorea in Huntington disease in the United States. Presented at: Annual Psych Congress; October 29-November 2, 2024; Boston, MA. 13. DrugBank Online. P-glycoprotein substrates. Accessed March 25, 2025. https://go.drugbank.com/categories/DBCAT002668 14. Ingrezza® (valbenazine) capsules. Prescribing Information. San Diego, CA: Neurocrine Biosciences, Inc. 15. Levi M, Schneider F, Gosselin NH, et al. Population pharmacokinetic and exposure safety analyses of deutetrabenazine in patients with moderate to severe tardive dyskinesia. Presented at: American Conference on Pharmacometrics; October 20-23, 2019; Orlando, FL. 16. Singh R, Sunzel EM, Dongwoo K, et al. Assessment of the deutetrabenazine exposure-response relationships for patients with moderate-to-severe tardive dyskinesia. Presented at: Psych Congress; September 17-20, 2022; New Orleans, LA.